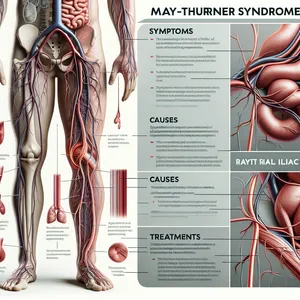
Understanding May-Thurner Syndrome: Definitions, Causes, and Symptoms
May-Thurner Syndrome is characterized by the compression of the left iliac vein by the right
iliac artery, a condition that can lead to serious venous disorders such as deep vein
thrombosis (DVT). While it remains underdiagnosed, understanding its causes, symptoms, and
potential complications is imperative for effective management and treatment.
May-Thurner Syndrome (MTS), also known as iliac vein compression syndrome, is a rarely
diagnosed condition that plays a significant role in non-traumatic DVTs in the left
extremity. The essence of the syndrome lies in the anatomical abnormality where the right
iliac artery compresses the left iliac vein against the lumbar spine, leading to a range of
venous outflow obstruction symptoms. The hallmark of MTS is the development of DVT,
presenting as leg pain, swelling, and occasionally, varicose veins or ulcers due to chronic
venous insufficiency.
The diagnosis of May-Thurner Syndrome is complex and requires a high index of suspicion,
especially in individuals who present with unprovoked left-sided DVT. Diagnostic imaging
techniques such as Doppler ultrasound, CT venography, and MR venography play critical roles
in identifying venous compression. Treatment options for MTS have evolved significantly,
with endovascular therapies such as stenting becoming the cornerstone of management.
Recent advancements in the understanding and treatment of May-Thurner Syndrome have opened
new avenues for patients. Stenting, for instance, has shown promising results in relieving
venous compression and preventing the recurrence of DVT. However, a multidisciplinary
approach integrating vascular surgery, interventional radiology, and coagulation expertise
is essential for optimizing patient outcomes. Furthermore, the rise of minimally invasive
surgeries has reduced recovery times and improved quality of life for individuals living
with MTS.
Awareness and early detection of May-Thurner Syndrome are paramount. Healthcare
professionals are encouraged to consider MTS in the differential diagnosis of unexplained
left-sided DVT, particularly in young patients or those without traditional risk factors for
venous thromboembolism. Additionally, patients with a history of MTS or DVT should be
educated about the condition, treatment options, and the importance of follow-up care to
monitor for potential complications.
Explore More
May-Thurner Syndrome is more than a vascular anomaly; it's a condition that demands
heightened awareness for early detection and treatment. With advancements in diagnostic
imaging and minimally invasive therapies, there is hope for individuals affected by MTS.
Awareness among healthcare providers and patients can lead to more timely diagnoses,
effective treatments, and better overall outcomes.